Scientific Calendar November 2023
Lightening workloads while fostering the rapid diagnosis of urinary tract infections
What makes urinary tract infections a driver of antimicrobial resistance (AMR)?
Time-consuming routine diagnostics
Empiric prescriptions
UTI-related smptoms (e.g. fever)
Skipping of UTI diagnostics
Treatment with phytopharmaca
Congratulations!
That's the correct answer!
Sorry! That´s not completely correct!
Please try again
Sorry! That's not the correct answer!
Please try again
Notice
Please select at least one answer
Case story
Lightening workloads while fostering the rapid diagnosis of urinary tract infections
Urinary tract infections cause significant workloads to diagnostic laboratories with up to 80% of the samples turning out to be UTI-negative. Classic UTI diagnostics is a long-lasting procedure, since urine cultures and antibiotic susceptibility tests have to be performed. The prescription of empiric antibiotics is often a consequence, fostering the rise of antimicrobial resistances [R32-1].
Various investigations on the analytical performance have demonstrated the potential of the UF-Series to rule-out UTI by the absence of bacteriuria with potential impact on workflows and microbiological workloads [e.g. R32-2]. Since an absence of bacteriuria is observed in the vast majority of suspected UTI specimen, this implies the absence of a bacterial UTI, eliminating the need for further diagnostic processing of these samples by urine culture.
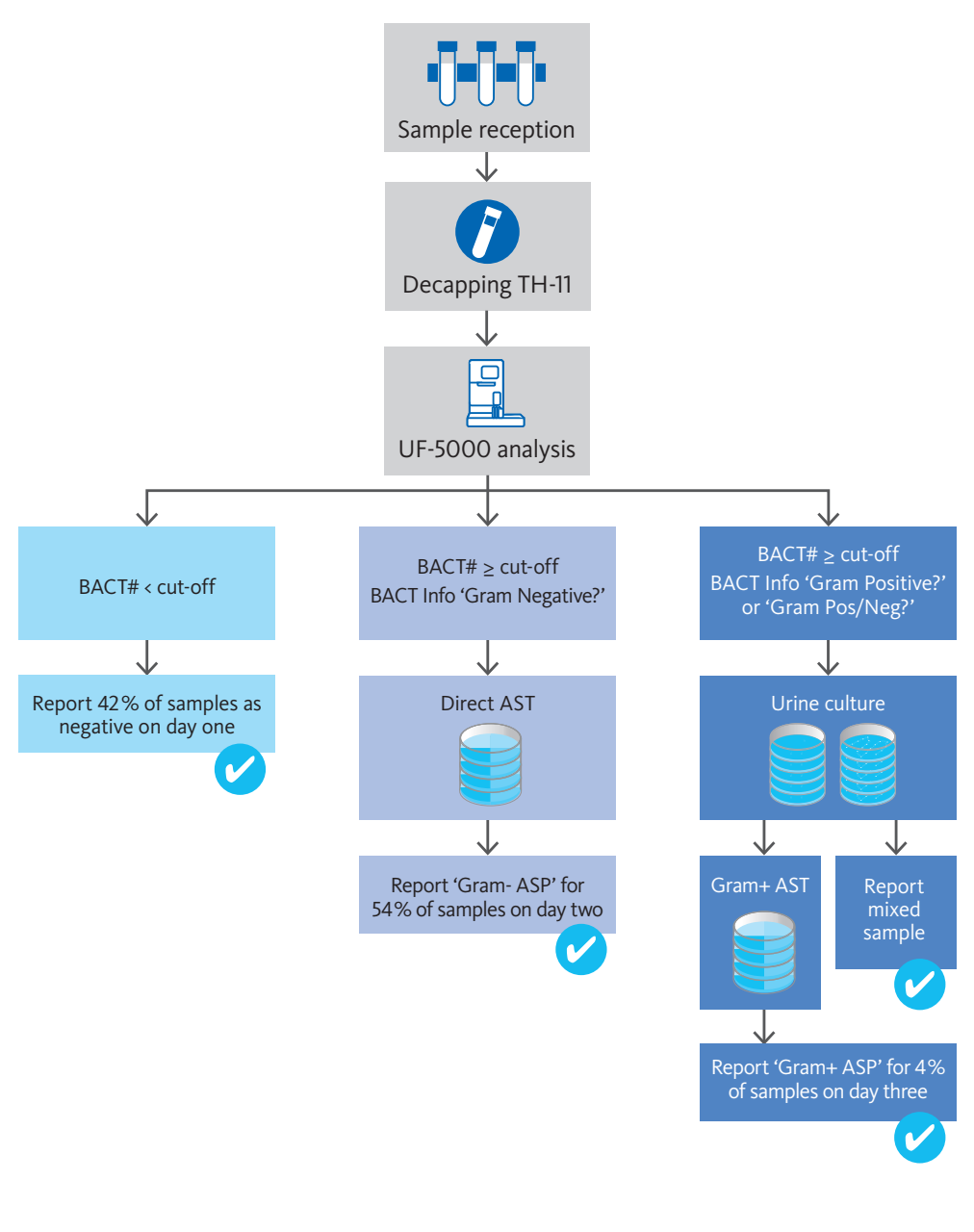
Gilboe et al. [R32-3] have demonstrated a significant potential of a combination of the bacteria and leucocyte count on the rule-out of UTI. Here, around 42% of all UTI-suspected samples can be directly reported as negative on the day of sample reception (Fig.1, left branch).
In addition, the potential impact of the ‘BACT Info’ flag on improving workflows and reporting times has been investigated. Here, the performance of the ‘Gram negative?’ flag in this setting allowed for urine culture to be skipped and for a direct antibiotic susceptibility testing (AST) approach to be conducted. This shortened the reporting time for antibiotic susceptibility profiles (ASP) for UTI-positive samples with Gram negative bacteriuria. In total, for 53% of the UTI samples, an ASP can be reported on the day after sample reception (Fig. 1, centre branch).
Only for UTI-positive samples with Gram positive bacteriuria (‘Gram positive?’) or mixed populations (‘Gram pos/neg?’) the full diagnostic pathway including urine culture was required. This, however, only affects a minority of the suspected UTI cases and for only 5% of the samples can an ASP be reported two days after sample reception (Fig.1, right branch).
This investigation highlights the potential of the UF-Series to reduce urine culture workloads and to improve workflow efficiency and reporting times by fostering a rapid diagnostics approach.
Depicted in the calendar image: Upper urinary tract infection
Upper urinary tract infections are a result of the ascencion of the pathogens from the bladder up into the ureter and the kidneys. Depending on the progression of the upper urinary tract infection, the infection is further differentiated into ureteritis, pyelonephritis and nephritis. Though an upper UTI is not per se defined as a complicated UTI, the differentiation of upper and lower urinary tract infection is of clinical relevance, since renal involvement correlates with more severe complications and clinical outcomes [R33-1].
With 13 and 3 cases per 10,000 UTI cases in women and men, respectively, the incidence of upper UTI is less than lower UTI [R33-2] and coincide with additional and more severe symptoms, such as pain and discomfort in the flanks, lower back or around the genitals, a high temperature, shivering or chills, fatigue and diarrhoea [R33-3].
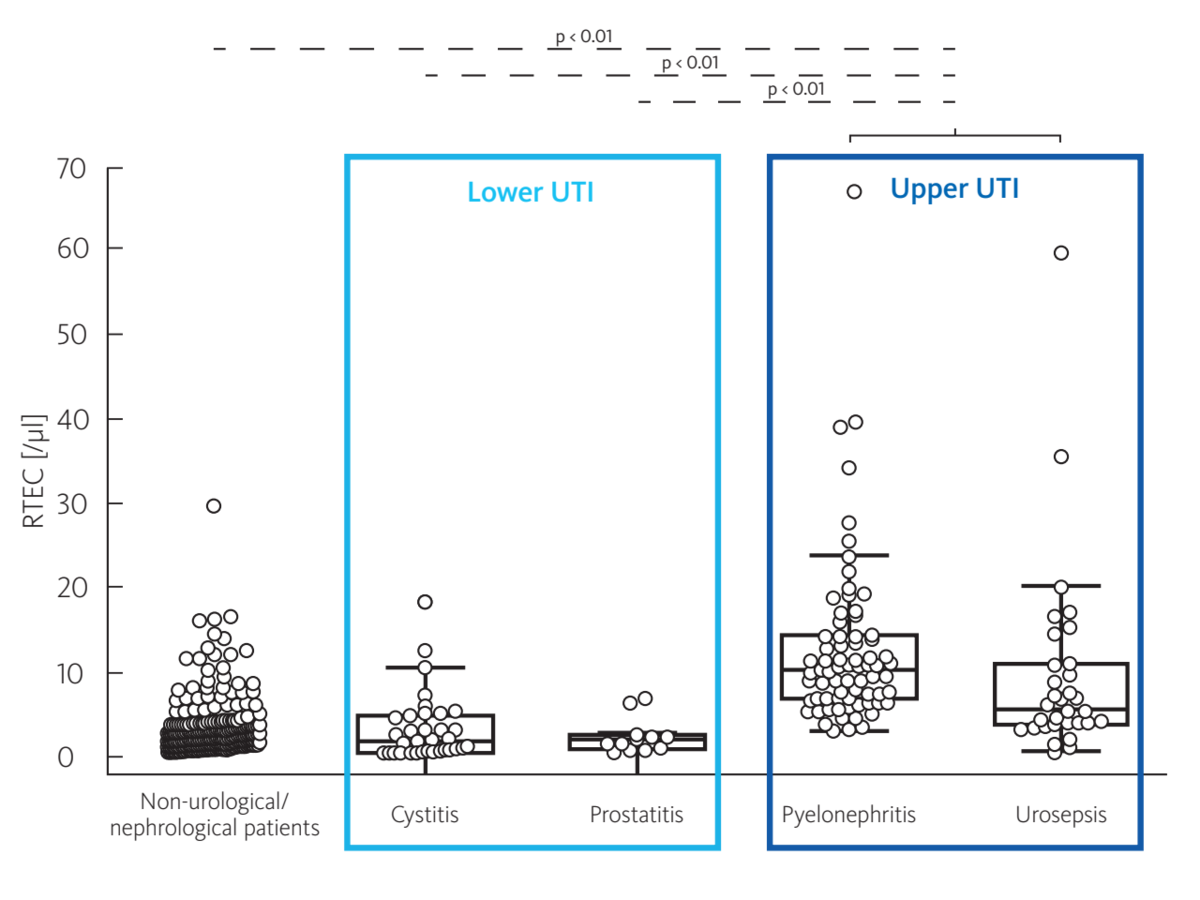
On the UF-Series, Oyaert et al. demonstrated the potential to differentiate between upper and lower urinary tract infection by utilisation of the RTEC parameter for the detection of renal tubular epithelial cells (Fig. 2). They concluded that in patients with a confirmed UTI, the presence of RTEC indicates an upper urinary tract infection. In these investigations, the diagnostic performance of this parameter outperformed classical markers of upper urinary tract infections, such as α1-microglobulin [R33-4].
Scientific background
Urinary tract infection (UTI) is one of the most common bacterial infections with around 400 million individuals (male and female) affected annually, worldwide [R31-1]. Female individuals are especially affected by this infection, as 60% of all women face a UTI at some point in their lives [R31-2] and 30-45% of females develop recurrent UTIs, defined as either within three months or within the subsequent year after the primary infection [R31-3].
The prevalence of UTI also accounts for a significant impact of this infection on healthcare systems and societies, as UTI accounts for millions of annual doctors visits [R31-4], significant workloads for clinical laboratories [R31-5] and for approximately 15% of all antibiotic prescriptions in the US and Europe [R31-6]. Among these antibiotic prescriptions, a great number of prescriptions are made empirically without proper diagnostics [R31-7]. Therefore, UTI can be considered a strong driver of antimicrobial resistance (AMR) [R31-8] and proper UTI diagnostics might help to support antimicrobial stewardship by avoiding unnecessary antibiotic prescriptions and fostering rapid and targeted treatments.
References
[1] R31-1 Yang X, Chen H, Zheng Y, Qu S, Wang H and Yi F (2022): Disease burden and long-term trends of urinary tract infections: A worldwide report. Front Public Health 10:888205.
[2] R31-2 Flores-Mireles AL, Walker JN, Caparon M and Hultgren SJ (2015): Urinary tract infections: epidemiology, mechanisms of infection and treatment options. Nat Rev Microbiol 13(5):269-84.
[3] R31-3 Gupta K and Trautner BW (2013): Diagnosis and management of recurrent urinary tract infections in non-pregnant women. BMJ 346:f3140.
[4] R31-4 Foxman B (2013): Urinary tract infection syndromes: occurrence, recurrence, bacteriology, risk factors, and disease burden. Infect Dis Clin North Am 28(1):1-13.
[5] R31-5 Wilson ML and Gaido L (2004): Laboratory diagnosis of urinary tract infections in adult patients. Clin Infect Dis 38(8):1150-8.
[6] R31-6 Foxman B (2002): Epidemiology of urinary tract infections: incidence, morbidity, and economic costs. Am J Med. 2002 Jul 8;113 Suppl 1A:5S-13S.
[7] R31-7 Pujades-Rodriguez M, West RM, Wilcox MH and Sandoe J (2019): Lower Urinary Tract Infections: Management, Outcomes and Risk Factors for Antibiotic Re-prescription in Primary Care. EClinicalMedicine 14:23-31.
[8] R31-8 O'Brien M, Marijam A, Mitrani-Gold FS, Terry L, Taylor-Stokes G and Joshi AV (2023): Unmet needs in uncomplicated urinary tract infection in the United States and Germany: a physician survey. BMC Infect Dis 23(1):281.
[9] R32-1 Keller P (2019): The next step towards faster urinalysis Sysmex Xtra article
[10] R32-2 De Rosa R, Grosso S, Lorenzi S, Bruschetta G, Camporese A (2018): Evaluation of the new Sysmex UF-5000 fluorescence flow cytometry analyser for ruling out bacterial urinary tract infection and for prediction of Gram-negative bacteria in urine cultures. Clinica Chimica Acta 484:171–178.
[11] R32-3 Gilboe HM, Reiakvam OM, Aasen L, Tjade T, Bjerner J, Ranheim TE and Gaustad P (2021): Rapid diagnosis and reduced workload for urinary tract infection using flowcytometry combined with direct antibiotic susceptibility testing. PLoS One 16(7):e0254064
[12] R33-1 Lane DR and Takhar SS (2011): Diagnosis and Management of Urinary Tract Infection and Pyelonephritis. Emerg Med Clin North Am 29(3):539–552.
[13] R33-2 Czaja CA, Scholes D, Hooton TM and Stamm WE (2007): Population-based epidemiologic analysis of acute pyelonephritis. Clin Infect Dis 45(3):273-80.
[14] R33-3 Hudson C and Mortimore G (2020): The diagnosis and management of a patient with acute pyelonephritis. Br J Nurs 29(3):144-150.
[15] R33-4 Oyaert M, Speeckaert M, Boelens J, Delanghe JR (2020): Renal tubular epithelial cells add value in the diagnosis of upper urinary tract pathology. Clin Chem Lab Med 58(4):597–604.