Scientific Calendar November 2020
How are neoplastic lymphocytes detected in the WPC measurement channel?
Cell membranes of neoplastic lymphocytes are more mature and more readily permeated, causing higher fluorescence signals.
The cell membranes are slightly perforated while leaving the cells largely intact. The fluorescence marker labels the intracellular nucleic acids (mainly RNA).
The side scattered light signals of neoplastic lymphocytes are lower than those of other white blood cells.
Congratulations!
That's the correct answer!
Sorry! That´s not completely correct!
Please try again
Sorry! That's not the correct answer!
Please try again
Notice
Please select at least one answer
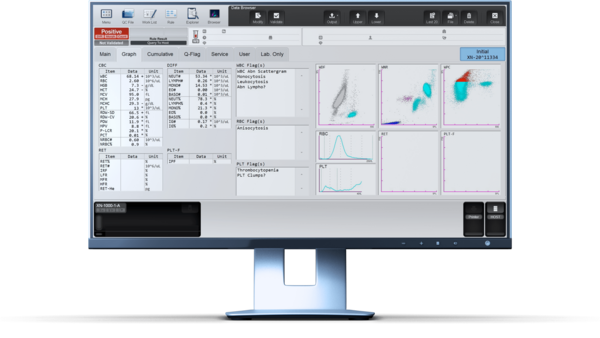
Numerical results
A peripheral blood sample of a 60-year-old man without medical history was investigated in the laboratory. The patient’s family history includes a Hodgkin lymphoma diagnosis of the mother. The analysis revealed marked leucocytosis together with anaemia (HGB = 73 g/L or 4.5 mmol/L) and severe thrombocytopenia (PLT = 13 x109/L). Out of a new blood sample, a second measurement including PLT-F channel confirmed the severe thrombocytopenia with a platelet result of PLT-F = 8 x109/L.The question in such cases is always whether the lymphocytes are of a reactive or neoplastic origin.
Scattergram interpretation
Using the CBC+DIFF measurement profile on an XN analyser, the white blood cells are counted in the WNR measurement channel and differentiated in the WDF measurement channel. In this patient’s WDF scattergram, the WBC subpopulations could not be clearly separated, which lead to the flag message ‘Blasts/Abn Lympho?’. Both reactive lymphocytes and lymphoma cells show increased fluorescence (see grey cluster).
An additional measurement channel to identify white precursor and pathological cells is the WPC channel which uses a specific set of reagents that influence the permeabilisation of the cell membrane. This advanced technology allows separating suspected malignant cells from healthy ones.
A high degree of membrane damage caused by the WPC lysing reagent leads to cellular components leaking through the pores, resulting in a decreased cell size. Additionally, more fluorescence marker can enter the cell and so bind even to nuclear DNA, which in turn leads to a higher fluorescence signal intensity. Neoplastic lymphocytes are more mature in their membrane structure than, for example, blast cells and are therefore more readily permeated, causing higher fluorescence signals. In this case example, the flag message ‘Abn Lympho?’ was triggered, which is suspicious of neoplastic lymphocytes.
Subsequent flow cytometric analysis confirmed a large monoclonal B cell population with the phenotype fitting to a mantle cell lymphoma (see detailed results below).
Immunophenotyping results
The absolute number of monoclonal B cells was 57.59 x109/L with 91% lymphocytes, 0.2% CD3+ T cells, 0.1% NK cells. The CD4/CD8 ratio was 2.0.
91% abnormal CD19+ B cells with this phenotype: Kappa++, CD19+, CD20++, CD5+, CD38zw+, FMC7+, CD79b+, CD43-, CD10-, CD200-, monoclonal K/L ratio: >10, CD23 possibly weakly positive (high background).
Also, the bone marrow biopsy showed that about 70% of BM was taken up by a small B cell non-Hodgkin lymphoma which was immunohistochemically most coherent with mantle cell lymphoma.
References
[1] Fact sheet ‘Mantle Cell Lymphoma’ from lymphoma.org. Access date 03.09.2020.
[2] Swerdlow SH et al. (2016) The 2016 revision of the World Health Organization classification of lymphoid neoplasms. Blood, 127(20): 2375–2390. https://doi.org/10.1182/blood-2016-01-643569.
[3] SEED ‘Lymphocyte differentiation update – helpful or dispensable?’
[4] Sysmex white paper ‘Going beyond the visible: Reliable characterisation of WBC functionality.’
Scientific background
The mantle cell lymphoma (MCL) is a specific lymphoma type and the most common cause for blood cancer [1]. Lymphomas are characterised by the uncontrolled proliferation of lymphocytes, a subgroup of white blood cells, and form a heterogeneous group of disorders.
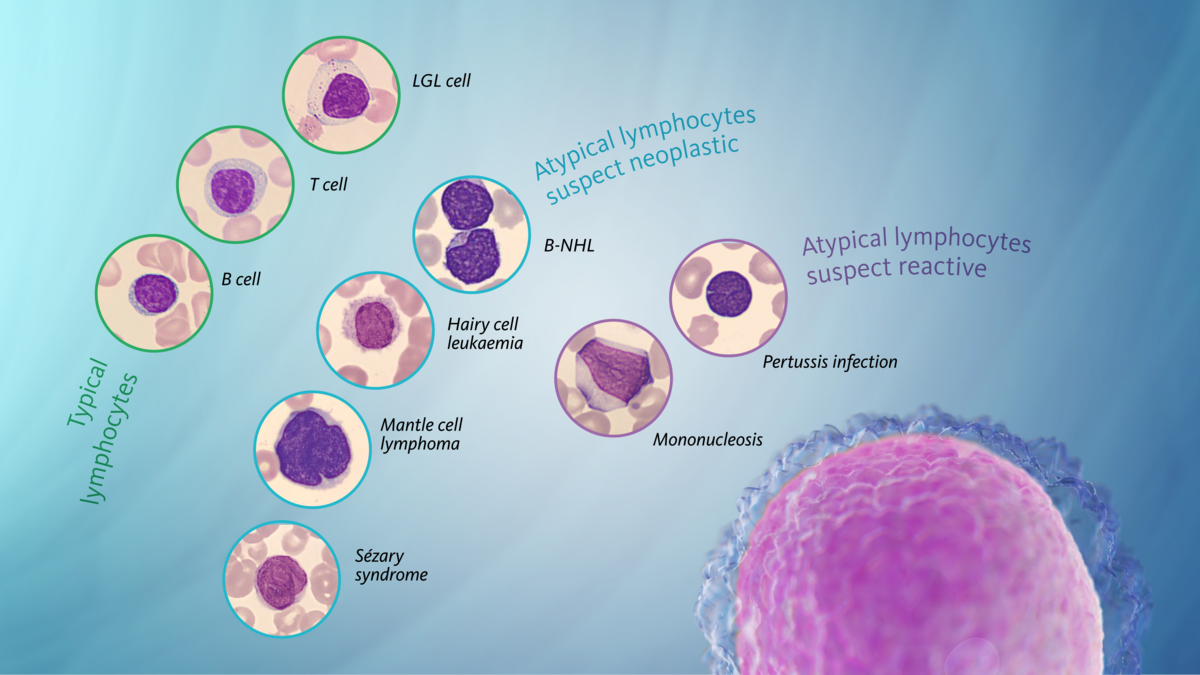
In the human body, different subgroups of lymphocytes exist, with T cells and B cells among them. Lymphomas, caused by malignant B cells and/or T cells, are divided into Hodgkin lymphoma (HL) and non-Hodgkin lymphoma (NHL). The mantle cell lymphoma is a rare B cell lymphoma and therefore belongs to the group of NHL [1].
The name ‘mantle cell lymphoma’ derives from the aetiology of the malignant cells, which originate from the mantle zone of the lymph node. These neoplastic B cells travel through the body and form peripheral tumour masses. The disorder is considered aggressive and fast progressing. According to the WHO lymphoma classification, a second, indolent (slowly developing) type of mantle cell lymphoma exists but is also incurable and may develop into the aggressive form [2].
The increased number of neoplastic lymphocytes in the patients’ blood shows up in a complete blood count and therefore leads to a further differential diagnostic procedure until the final diagnosis is secured.
One of the biggest challenges in cytology is the differentiation of lymphocytes in blood films because they appear in many varieties, and diseases are manifold. Aside from the experience of the examiner, the basis for qualified cytological blood findings is the availability of a standardised nomenclature, especially in cases where there are lymphocyte alterations. Lymphocytes of an unusual appearance can be released into peripheral blood due to reactive diseases (e.g. viral infections) and neoplasms (e.g. lymphomas). According to the lymphocyte classification 2011, these lymphocytes are described as ‘atypical’ regardless of their cause. Here, ‘atypical’ means that, when stained according to the Pappenheim method, these lymphocytes appear different from the typical lymphocytes or large granular lymphocyte (LGL) cells [3].
Immunophenotype characterisation, histological diagnostics and complementary cytogenetic and molecular genetic testing are essential for further cell classification and prognostic assessment.
By using an ingenious reagent system, Sysmex’s XN-Series analysers permit to differentiate cells by their functionality, overcoming limitations of morphological examination and allowing conclusions on
- the maturity of a cell,
- the malignancy of a cell, and
- the activation state of a cell [4].